Garment Originally Made for Astronauts is Saving Lives of New Mothers in Developing Countries
LifeWrap
"It’s simple, reusable and affordable.”
In 1969, medical researchers at NASA’s Ames Research Center were referred an unusual patient: a local California woman who had given birth to a healthy baby, but who kept hemorrhaging dangerous amounts of blood.
While doctors at Stanford University Hospital gave the hemorrhage patient a blood transfusion, engineers at the space agency brainstormed solutions to stop the bleeding. They decided to try an anti-gravity suit—typically used to keep astronauts from blacking out during extreme acceleration by squeezing the arms and legs to push blood back toward the head—to apply external pressure to the woman’s lower body and drive blood upward. It was a success, and the woman’s life was saved.
Soon after, a version of the suit was created for battlefield injuries affecting the lower body. The half-suit, using elastic compression and not the pneumatic compression used in the astronaut version. was applied as an emergency rescue measure to stabilize soldiers suffering from shock. In 2001, Stanford obstetrician Paul Hensleigh tested the garment in a hospital setting: he was able to save the lives of 13 out of 14 patients in shock from extreme blood loss in a facility in Pakistan.
Taking inspiration from NASA and Hensleigh’s research, Suellen Miller, the founder of University of California San Francisco’s Safe Motherhood Program, set out to adapt the technology to treat new mothers who slip into shock because of excessive bleeding. It’s a particular problem in the developing world, where postpartum hemorrhage—loss of more than 500 milliliters of blood after the birth of a baby—accounts for 60 percent of maternal mortality cases.
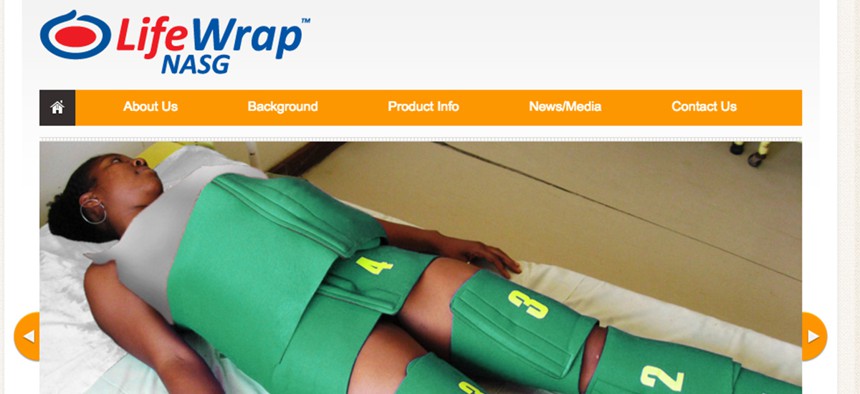
Together with Hensleigh, Miller created a non-pneumatic anti-shock garment that applies pressure on the lower half of the body to push blood to vital organs like the lungs, heart and brain. The wetsuit-like contraption, which has since been christened LifeWrap, is made of a synthetic rubber called neoprene and uses Velcro fastenings to alter the pressure applied.
The anti-shock garment is a first-aid measure: Strapping on LifeWrap soon after giving birth can help contain or at least slow down excess bleeding. Typically, clinicians will administer oxytocin to stop the blood loss. If the drug is not available or is ineffective, nurses and doctors can use the NASG to buy more time.
In 2003, Hensleigh and Miller got a grant from the MacArthur foundation to conduct clinical trials. They began with a 6-month pilot in Egypt: From May to August 2004, they measured blood loss from 158 PPH patients who received standard care. Then, from September to December 2004, they measured the blood loss for 206 patients treated with the NASG. Results showed the suit cut maternal mortality rates by over 50 percent.
However, Miller and her team recognized that testing in one or two countries showed strong correlation but not causation—other external factors could have caused maternal mortality rates to drop. To make sure the results were as robust across different conditions, they did more trials: Between 2004 and 2007, further tests in Egypt and Nigeria yielded similar results—as did randomized cluster trials in Zambia and Zimbabwe from 2007 to 2013.
In areas where maternal mortality rates were especially abysmal to begin with, improvement was even more significant. In 2013, the World Health Organization added the anti-shock garment to its PPH treatment guidelines.
“Nobody thought of using [the technology] in this very dire situation for women globally,” Miller says. “It’s simple, reusable and affordable.”
Typically, the garment costs around $55, but many low-income countries part of the United Nation’s Life Saving Commodities group, established by the UN Population Fund to help scale technologies to save 16 million women and children by 2015, pay closer to $42. If washed and preserved in optimal condition, each garment can be used over 100 times—that brings the cost of use per birth down to well under $1.
The potential impact of the NASG is huge. In many of the countries where LifeWrap has been deployed, there are hundreds and thousands of maternal deaths per 100,000 births. (By way of comparison, the U.S. rate in 2015 was 14 per 100,000.)

Even in richer countries, LifeWrap can be a useful tool in situations like addressing complications in rural areas or during home births, Miller says.
“It’s so safe—there are absolutely no adverse outcomes, no bad side effects,” she says. “I’d like to see it everywhere. Every ambulance, every facility, every midwife, every doctor should have one because they’re going to be able to save lives.”

“It’s extremely easy and and in some ways even very self-explanatory,” says Farouk Jega, the Nigeria director of international nonprofit Pathfinder, which works to deploy the life-saving garment across the country. Anyone can apply a LifeWrap—no need for an obstetrician, nurse, or midwife to be present.
“All you require is to do it quickly,” Jega says. “We have even trained ambulance drivers for emergencies [in Nigeria].” The south Indian state of Tamil Nadu has done the same. (There are plans to scale the product to other states across India.)
But Jega warns there’s a risk of politicians touting the garment as a silver bullet for maternal mortality, and avoiding addressing deeper infrastructural problems.
“We need to make sure there are enough health care providers and ensure ready supply for blood banks in a facility all year around,” he says.
While developing nations work to improve their medical facilities, train health care professionals and make other institutional changes, the anti-shock garment could become an essential stopgap.





